What is the new variant HKU1 Covid-19 variant?
This case study is the first to describe symptomatic pneumonia associated with HKU1 variant following combined anti-CTLA and anti-PD-1 blockade with ipilimumab and nivolumab in patients with metastatic melanoma.
What are the symptoms of HKU1 variant?
Adults have respiratory symptoms, most commonly shortness of breath, cough, and runny nose. Among 19 critically ill hospitalized patients, HCV OC43-NP (P = 0.016) and HKU1-NP HKU1-NP (P = 0.023) antibody levels were significantly lower at the first visit compared with other COVID-19 patients.
This biomarker study demonstrated that prior exposure to HCV OC43 and HKU1 was more strongly associated with COVID-19 severity than prior HCV 229E or NL63 infection. To further assess the potential clinical significance of antibodies against epidemic coronavirus in COVID-19 patients, the correlation of Los with anti-HCV OC43 and HKU1 antibody levels was analyzed (Figure 2).
The common coronavirus, called the OC43 antibody, does not bind to the S1 region of the SARS-CoV-2 peak and cannot prevent SARS-CoV-2 from entering cells. His team found that serum samples from people before the pandemic contained an antibody against the common cold coronavirus called OC43 that binds to the common cold coronavirus’ SARS-CoV-22 spike protein. OC43 (the spike protein of SARS-CoV) binding. Twenty-two.
The receipt was changed in 2002 when cases of severe SARS were reported in Guangdong, China, causing global concern as the disease spread through international travel to more than 2 dozen countries.2 The new illness became known as Severe acute respiratory syndrome. (SARS), and a beta HCoV called SARS-CoV has been identified as the causative agent.
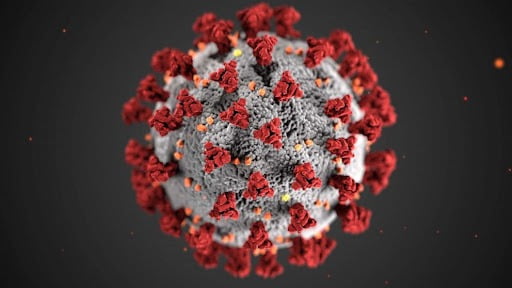
As the name suggests, the virus is related to the SARS-associated coronavirus (SARS-CoV) that caused the severe acute respiratory syndrome (SARS) outbreak in 2002-2003, but it is not the same virus. In the 21st century, two highly pathogenic HCVs—severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV)—have emerged from animal reservoirs, causing global epidemics with morbidity and alarming mortality. Human coronaviruses (CoV) have long been recognized as a common cause of the respiratory disease: the first reports of CoV 229E and CoV OC43 as the cause of the common cold in adults appeared in the mid-1960s [1].
For SARS-CoV-2, there is growing evidence that exposure to other coronaviruses, including those that cause colds and other respiratory illnesses, plays a role in people’s immune responses. MERS-CoV has various clinical manifestations from mild to moderate to severe, and some patients develop acute respiratory distress syndrome (ARDS).
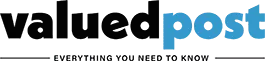
Epidemiology of human coronavirus infection NL63 in hospitalized patients with pneumonia in Taiwan. Opens in a new tab Download slideshow Anterior-posterior (AP) chest radiograph of an adult admitted to hospital with coronavirus respiratory disease (CoV)-HKU1 Coronavirus-associated respiratory disease (CoV)-HKU1. As of May 6, 2020, novel COVID-19 has been confirmed in more than 3,500,000 patients worldwide, with a mortality rate of approximately 6.8%. Figure 19 shows a two-phase flow.