What is black fungus?
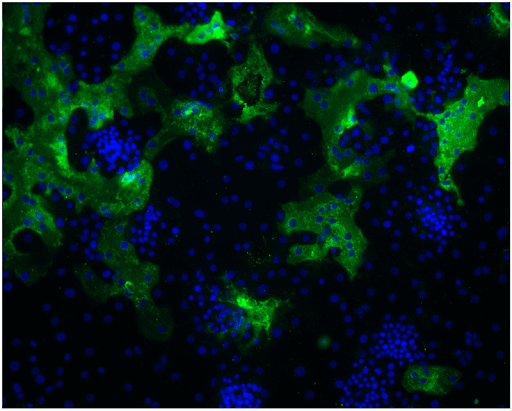
Mucormycosis is also known as black fungus, a rare fungal infection that transpires when exposed to fungi named mucormycetes. These fungi occur in the atmosphere usually in soil, leaves, animal dung, and compost. Mucormycetes penetrate the body during inhaling, breathing, and exposed wounds in the skin. There are several kinds of mucormycosis pulmonary (lung), rhinocerebral (sinus and brain), cutaneous (skin), and gastrointestinal mucormycosis.
The symptoms related to skin, which can occur and spread in any part of the body, are-
- blackened skin tissue
- redness, swelling, tenderness
- blisters
- ulcers
The symptoms related to respiration are-
- cough
- fever
- headache
- chest pain
- nasal or sinus congestion and pain
- shortness of breath
This fungal infection is not contagious. Moreover, who come in touch with fungi do not receive an infection. However, people with weak immune system have a high risk of getting mucormycosis. This includes people suffering from-
- diabetes
- cancer
- HIV
- skin injury
- surgery
Doctors can treat this infection by applying and managing antifungal medication. They even might have to perform surgery to evacuate the affected area. According to the Centers for Disease Control and Prevention (CDC), if this disease is left untreated, mucormycosis can become dangerous, leaving the person with a mortality rate of only 54%.
you may also read: the rise of covid-19 strikes again
What causes mucormycosis?
Mucormycosis is known as black fungus or zygomycosis. Mucormycetes are a group of molds that give rise to this disease. According to the Center for Disease Control and Prevention, these fungi reside in the environment. They specifically live in a dead and decaying matter like leaves, compost, rotten wood, and soil. If an individual breathes these fungal pores, they might acquire the infection commonly affecting the sinuses or lungs. The specialists say that this infection is an opportunistic infection. It latches on to those going through any sickness. Experts say that those suffering from Covid-19 have weak immunity, and most of them are given steroids to control hyperimmune response. This process makes them responsive to other infections like mucormycosis.
Most mucormycosis infections are found in Covid-19 patients with diabetes or those with underlying and undetected high blood sugar.
The poor quality of air in India and extreme dust in cities like Mumbai make it more hospitable for the fungi to survive and spread. Navalakhe said that there is an excessive misapplication and overuse of steroids and antibiotics in India, due to which the infections spread at a large scale.
Is Mucormycosis contagious?
The disease is NOT contagious! It cannot transfer through direct contact between humans or animals. It spreads from the fungal spores present in the air or environment, which is not easy but is impossible to avoid. Head of Narayana Nethralaya, a speciality eye hospital, K Bhujang Shetty, said bacteria and fungi exist in our bodies. But, our immune system keeps them in control. He also said that when the immune system weakens due to cancer, diabetes, or steroids, these organisms get a head start, and they start to spread in the body.
Why is it occurring in COVID 19 patients?
Mucormycosis can happen anytime after suffering from Covid-19 infection. It can occur either while staying in the hospital or several days to a few weeks after getting discharged.
Covid-19 causes beneficial changes in the host’s internal environment suitable for the fungus and the medical treatment provided, unconsciously encouraging fungal growth. Coronavirus destroys the blood vessels and the airway mucosa.
It leads to an increment in the serum iron necessary for the fungus to spread. The medications such as steroids lead to a rise in blood sugar—the broadspectrum wipes out the potentially pathogenic bacteria and the protective commensals. Some antifungals, such as Voriconazole, hinder Aspergillosis, but
Mucor survives unharmed and spreads as there is no competition to fight with. Using ventilation for the long term lessens the immunity. There are considerations that the fungus can transmit by the humidifier water supplied and the oxygen. All these steps make the mucormycosis infection spread.

Treatment of Covid-associated Mucormycosis
Uncontrolled diabetes or ill-usage of steroids in immunocompromised patients often gives rise to Mucormycosis. Therefore, it is essential to control diabetes first, maintain steroids-its time, dose, and usage- and stop using other immunomodulation drugs. People with diabetes and non-diabetic patients must control hyperglycemia (high sugar levels). Mostly when they have been discharged after the Covid-19 treatment.
In the early stages of Mucormycosis, It is possible to treat Mucormycosis with a suitable antifungal treatment. In some cases, surgical debridement is required to eliminate the necrotic material off the skin. A team that includes microbiologists, infectious disease specialists, dentists, surgeons, histopathologists, neurologists, and radiologists is necessary.
sourced by: fungal diseases and covid-19